Posture, balance, and coordination are three pillars of school-based physical therapy.
Ensuring these systems are functional allows our students to engage with their school environment. I always love seeing how other therapists address these key elements, so I figured it was my turn to share!
Posture
Posture is analyzed statically and dynamically in a school setting. Statically, we may examine seating ergonomics in the classroom. Dynamically, we analyze body alignment during mobility.
Low muscle tone and prolonged positioning (think Down Syndrome, Autism, iPad-lovers) contribute to head-down or head-forward posture. This postural misalignment is problematic for environmental obstacle scanning and social engagement. The former leads to falls and bumping into objects.
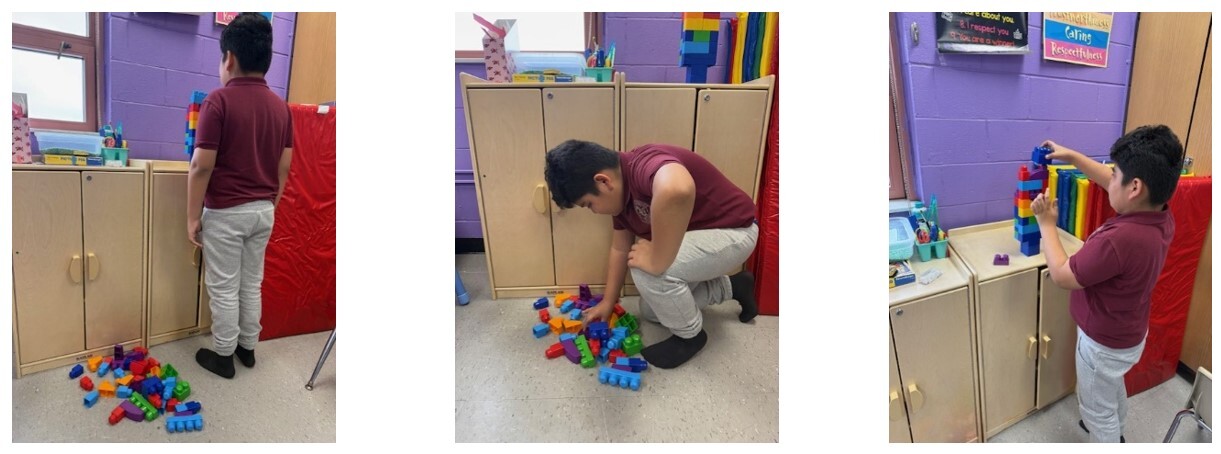
Intervention: Student picks up a block from the floor and places it on a higher surface. Ideally, they should place the objects around eye level or higher to facilitate forward and upward gaze.
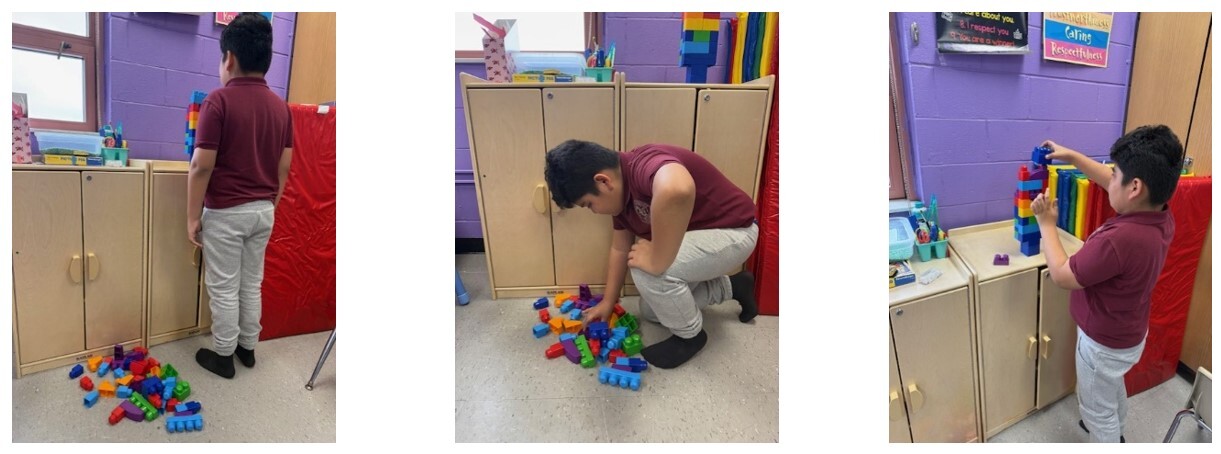
Clinical Reasoning: Changing levels to a higher surface require active neck extension. Placing the object at eye level or higher eliminates head-down posture. I like to use building blocks for this activity because the target gets gradually higher.
Progression: Standing on unstable surface, crossing midline
Regression: Less distance between levels
Coordination
Coordination can encompass a broad number of skills. People most commonly think of ball games like throw, catch, and kicking. For school-based PT services, it is also important to consider reciprocal movements (i.e. arm swing during running), motor dual-tasking (i.e. carry object while walking), upper/lower extremity connection, and movement corrections. I’ve included an activity that addresses coordination between the upper and lower extremities.
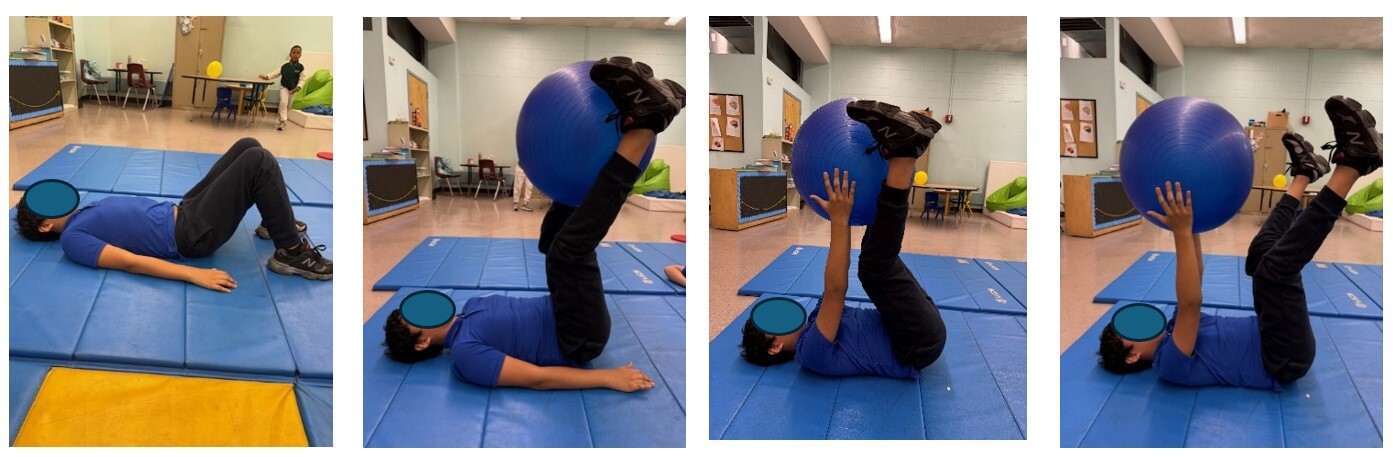
Intervention: Student starts in hook-lying or supine position. The ball is either placed or rolled between their feet. Using their lower extremities, they raise the ball and grab it with their hands. Then release the ball with their legs and move the ball overhead.
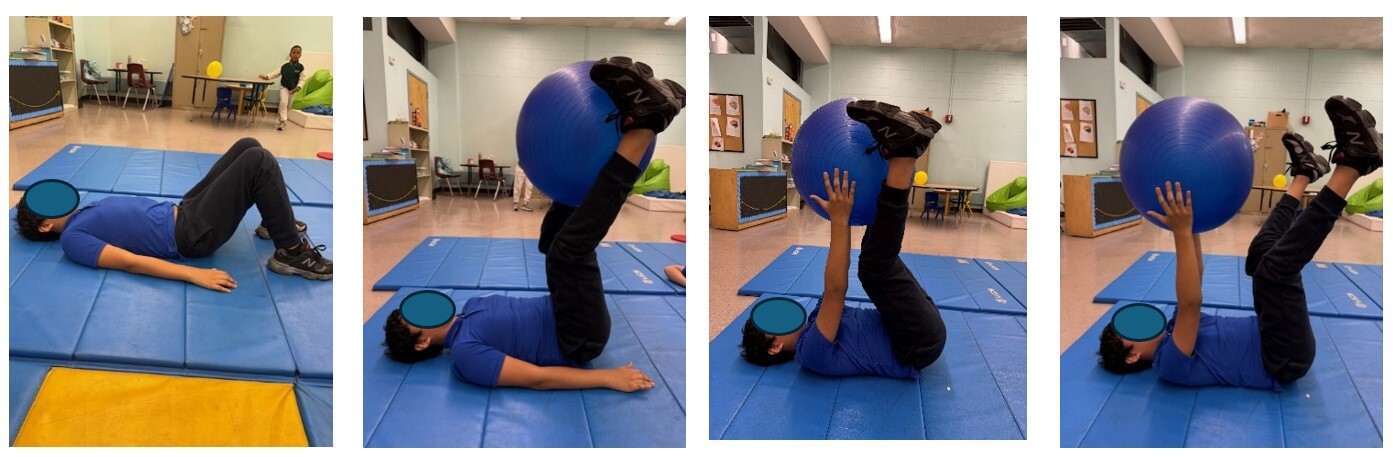
Clinical reasoning: Requires synchronized movement between upper and lower extremities to complete task. Movement requires significant core engagement as well – which facilitates proximal control necessary for distal control.
Progression: Use small ball, incorporate crossing planes of motion
Regression: Hold ball statically between knees and hands in reverse quadruped position.
Balance
The prevalence of balance disorders in children and adolescents is reported up to 15%. While some falls are inevitable during development, we strive for our students to play safely. Some things to consider are vestibular function, single limb stability, righting reactions, protective reactions, and proprioception.
Intervention: Student scoops up bean bags onto the top of their foot. Then they need to drop the bean bag off into designated area or bucket.

Clinical reasoning: Single limb stability needed for stair negotiation and stance phase of gait. This activity also promotes increased ankle dorsiflexion needed for foot clearance during swing phase.
Progression: Student stands on unstable surface, drop-off farther away requires leg reach beyond limb length
Regression: Support surface or handheld assistance for balance
Author: Cara Jenson, PT, DPT